By Cara Richmond
•
February 25, 2025
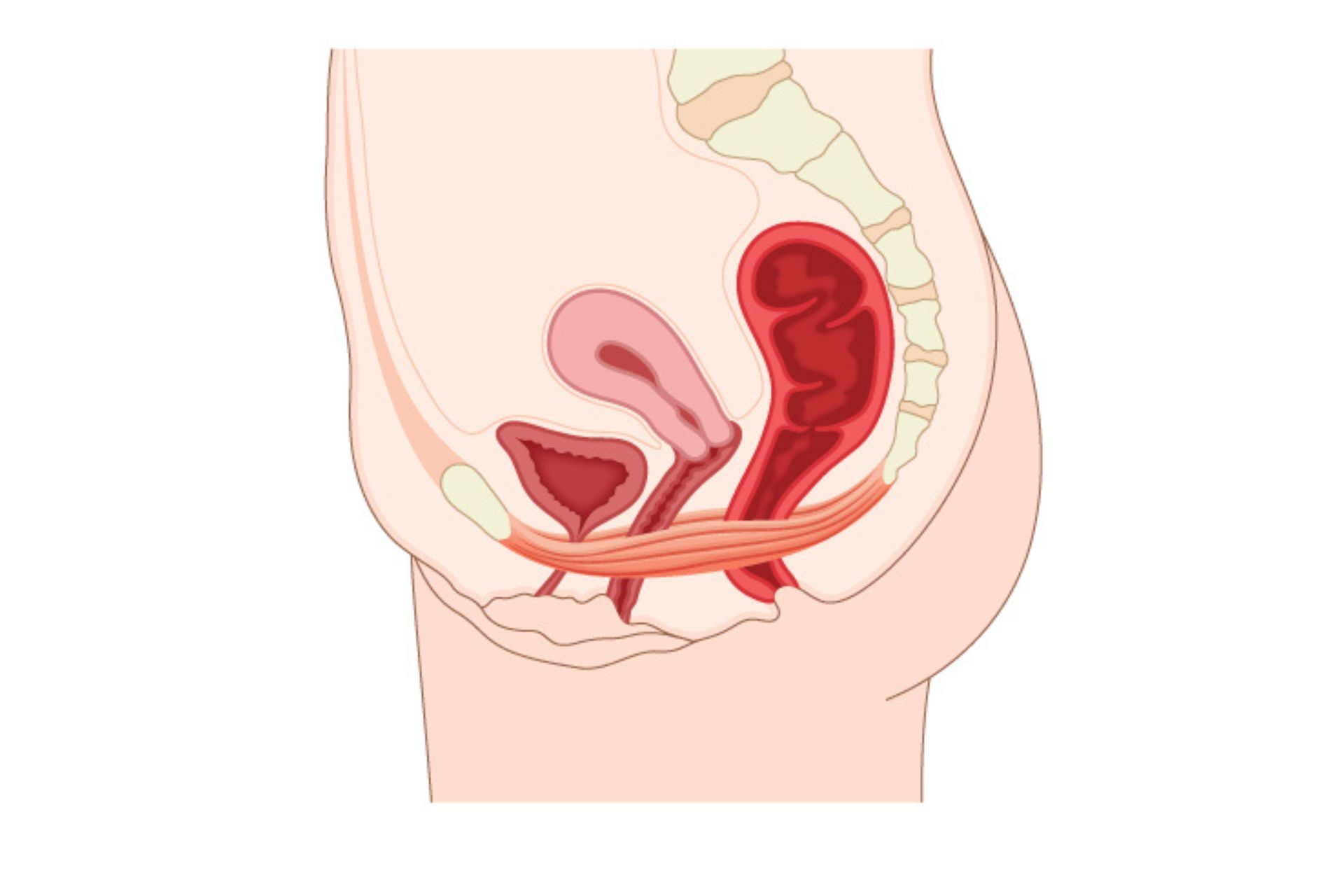
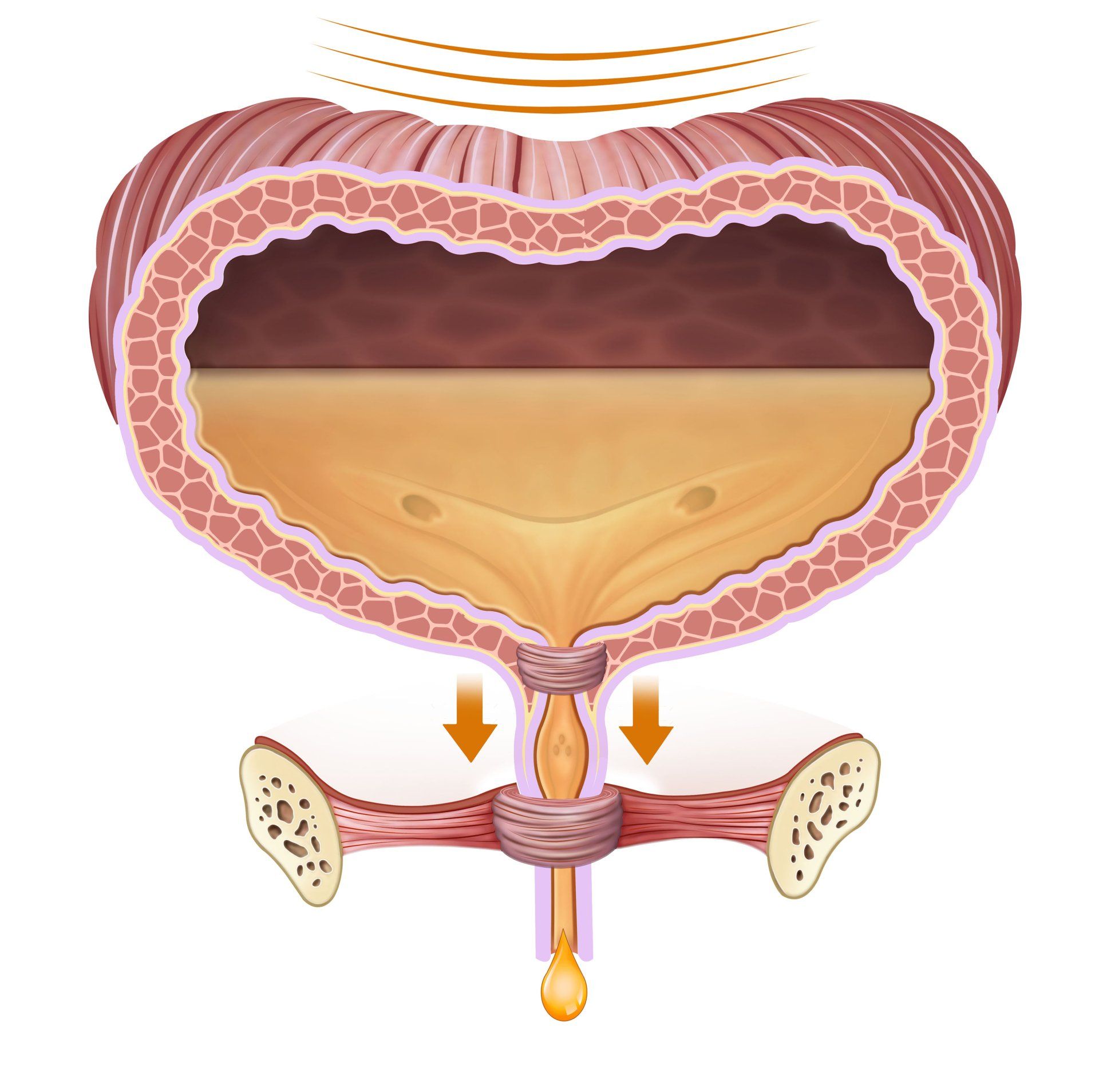
Endometriosis and adenomyosis are two common yet often misunderstood conditions that affect many individuals with uteruses, causing chronic pelvic pain, heavy periods, and various other symptoms. While traditional treatment approaches may focus on medication or surgical interventions, pelvic physiotherapy has proven to be an effective complementary treatment that helps manage pain, improve quality of life, and support overall pelvic health. In this blog, we will explore how pelvic physiotherapy can help individuals suffering from endometriosis and adenomyosis, offering relief and a holistic approach to managing these conditions. What Are Endometriosis and Adenomyosis? Before delving into how pelvic physiotherapy can help, it’s important to understand what endometriosis and adenomyosis are. Endometriosis occurs when tissue similar to the lining inside the uterus (the endometrium) grows outside the uterus, causing inflammation, scar tissue (adhesions), and often severe pelvic pain, particularly during menstruation. This condition can also affect fertility and cause painful intercourse. Adenomyosis happens when endometrial tissue grows into the muscular wall of the uterus. This can lead to an enlarged uterus, heavy and painful periods, pelvic pain, and even bloating or pressure in the lower abdomen. Unlike endometriosis, adenomyosis is confined to the uterus, but it can cause similarly debilitating symptoms. Both conditions can significantly affect daily life, leading to discomfort, fatigue, and emotional strain. However, pelvic physiotherapy offers a multifaceted approach that helps address the physical symptoms of these disorders. How Pelvic Physiotherapy Can Help Manage Endometriosis and Adenomyosis Pelvic physiotherapy focuses on the muscles, ligaments, and tissues in the pelvic region, with the aim of improving mobility, relieving pain, and restoring pelvic floor function. For individuals with endometriosis and adenomyosis, pelvic physiotherapists can use a range of techniques tailored to their specific symptoms and needs. Here’s how pelvic physiotherapy can offer relief: 1. Reducing Pelvic Pain One of the most common symptoms of both endometriosis and adenomyosis is chronic pelvic pain. Pelvic physiotherapists are trained to use a variety of hands-on techniques such as myofascial release, deep tissue massage, and trigger point therapy to reduce muscle tension in the pelvic floor and surrounding areas. These techniques help relax tight muscles, release scar tissue, and improve blood circulation, which can alleviate pain and reduce muscle spasms. For endometriosis, this is especially important, as the condition can cause deep pain, especially around the pelvic organs. By targeting these tight and tender areas, pelvic physiotherapy can help reduce the intensity and frequency of pain episodes. 2. Improving Pelvic Floor Function Both endometriosis and adenomyosis can affect the pelvic floor muscles, which play a critical role in bowel, bladder, and sexual function. Individuals with these conditions may experience pelvic floor dysfunction, which can manifest as pain during intercourse, urinary urgency, or constipation. Pelvic physiotherapy helps restore proper pelvic floor muscle function by teaching exercises that encourage both strengthening and relaxation of these muscles. This can improve bladder and bowel control, ease pain during intimacy, and restore normal pelvic muscle coordination, which may be compromised due to the ongoing pain and tension associated with these conditions. 3. Reducing Scar Tissue and Adhesions In endometriosis, the tissue that grows outside the uterus can form adhesions (scar tissue) that cause organs to stick together. This can lead to restricted movement, pain, and discomfort. Pelvic physiotherapists use manual therapy techniques to help break down or mobilize adhesions, improving organ mobility and reducing pain caused by these adhesions. While manual therapy cannot eliminate adhesions entirely, it can help improve flexibility and prevent further damage from forming. For individuals with adenomyosis, pelvic physiotherapy may not directly treat the condition itself, but it can address the resulting muscle stiffness and tension in the pelvic region caused by the uterine enlargement and pressure. 4. Helping with Menstrual Pain Management Pelvic physiotherapists often guide individuals through relaxation techniques and breathing exercises that help manage the cramping and pain associated with menstruation. By teaching individuals how to relax their pelvic muscles and focus on controlled breathing, physiotherapists can help minimise the intensity of menstrual cramps and reduce overall discomfort during the menstrual cycle. In addition, some pelvic physiotherapists work with individuals to create tailored exercise programs that help strengthen the core and pelvic muscles, which can aid in reducing menstrual pain over time. 5. Improving Posture and Pelvic Alignment Chronic pain from endometriosis and adenomyosis can lead to poor posture and abnormal pelvic alignment. Pelvic physiotherapists evaluate how these conditions affect posture and body mechanics and provide exercises to improve alignment. Correcting posture and body mechanics can reduce pain and strain on the pelvis, back, and hips, leading to better overall function and less discomfort during daily activities. 6. Providing Education and Lifestyle Modifications Pelvic physiotherapists offer education on how to manage day-to-day activities with less pain, including proper lifting techniques, postural adjustments, and movement modifications. They also provide advice on managing stress and anxiety, which can exacerbate pain and pelvic muscle tension. The Role of Pelvic Physiotherapy in a Holistic Treatment Plan Pelvic physiotherapy can be an important component of a comprehensive approach to managing endometriosis and adenomyosis. While it may not cure these conditions, it significantly improves quality of life by addressing the physical symptoms and offering strategies for pain relief. Combining pelvic physiotherapy with other treatments—such as medical management, hormone therapy, or even surgery—can provide a well-rounded approach to managing these chronic conditions. It is essential to consult with your healthcare provider before starting pelvic physiotherapy to ensure it’s part of an integrated treatment plan that works for you. Your physiotherapist can collaborate with your medical team to tailor the approach to your unique needs, ensuring the best possible outcome. Conclusion Pelvic physiotherapy offers a gentle, effective, and holistic approach to managing the chronic pain and pelvic dysfunction associated with endometriosis and adenomyosis. By targeting the pelvic floor muscles, releasing muscle tension, reducing adhesions, and improving overall pelvic function, physiotherapy can significantly improve your quality of life. If you are living with these conditions, consider discussing pelvic physiotherapy with your healthcare provider as part of your treatment plan. It might be the key to managing pain, restoring function, and regaining control over your life